A new generation of biological mapping technologies is radically changing how we understand and treat deadly diseases. Researchers are now able to study human tissue in unprecedented detail, pinpointing malfunctioning cells within organs and revealing the molecular mechanisms driving conditions previously considered incurable. This breakthrough, known as spatial multiomics, isn’t just refining existing treatments; it’s opening doors to entirely new therapies, particularly for conditions like toxic epidermal necrolysis (TEN), a severe skin reaction where patients literally shed their outer layer.
The Challenge of Complexity
For decades, medicine has approached disease by zooming in on organs, tissues, cells, and finally, the underlying molecules like DNA and proteins. However, this reductionist approach often misses crucial details. Even within a single organ, cells aren’t uniform; neighboring cells can behave differently, creating cascading damage that standard lab tools struggle to resolve. Traditional methods often “mash together” hundreds of cells for analysis, obscuring the critical changes happening at the individual level.
This complexity is especially acute in cancer, where researchers have long understood the “tumour microenvironment” — the idea that even under a microscope, a tumour isn’t uniform. But standard tools have struggled to pinpoint those differences.
The Rise of Spatial Multiomics
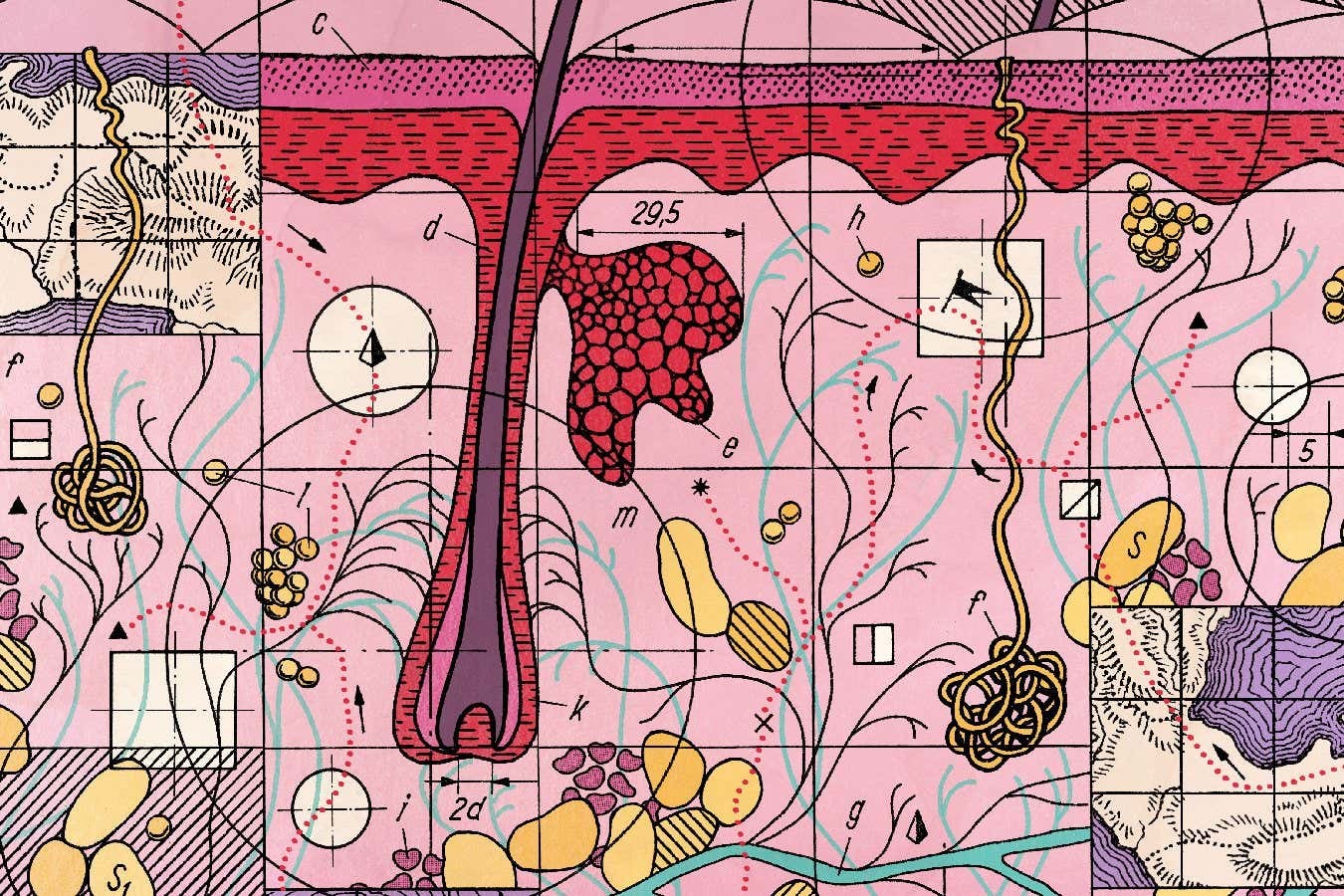
The key to unlocking this hidden detail lies in spatial multiomics, a suite of technologies that build three-dimensional maps of tissues and organs. These maps identify diseased cells and profile them at the molecular level, revealing exactly what has gone wrong in their biological machinery.
The term “multiomics” refers to studying multiple biological systems simultaneously: genes, RNA, proteins, and more. Spatial multiomics adds high-resolution imaging to this mix, allowing scientists to see not just what molecules are present, but where they are and how they interact across space.
One technique, “deep visual proteomics,” developed by researchers at the University of Copenhagen, involves slicing tissue into microscopic sections, staining them to highlight specific molecules, then using AI-powered microscopes to create detailed digital maps. A laser dissection microscope then cuts out labeled cells one by one, analyzing their proteins with extreme precision using mass spectrometry. The result is a molecular map that reveals the differences between healthy and abnormal cells, patterns of dysfunction that were previously invisible.
From Pancreatic Cancer to TEN: Real-World Applications
The potential of spatial multiomics extends far beyond theoretical research. Studies have already yielded crucial insights into conditions like pancreatic cancer, where researchers used this technology to identify early signs of tumor development in seemingly normal cells.
However, the most dramatic breakthrough has come in the treatment of toxic epidermal necrolysis (TEN), a rare but fatal skin condition where the immune system violently attacks the outer layer of skin. Dermatologist Thierry Nordmann’s team used spatial proteomics to uncover that the interferon pathway, normally activated by viral infections, was massively overactive in TEN patients, causing the immune system to destroy healthy skin cells.
Crucially, drugs already exist that block this pathway. In a small trial, seven TEN patients treated with these inhibitors showed remarkable recovery, with one patient regrowing almost all of his lost skin within 16 days. Nordmann believes this could become the standard treatment within two to three years.
The Future of Precision Medicine
Spatial multiomics isn’t cheap; running a few hundred samples can cost millions. But hospitals, like the Mayo Clinic, are already investing heavily in this technology, hoping to better understand conditions like heart disease and diabetes by identifying the cells most vulnerable to damage.
The implications are profound: spatial multiomics isn’t just refining existing treatments; it’s paving the way for a new era of precision medicine, where therapies are tailored to the unique molecular landscape of each patient’s disease. The ability to map and understand the inner workings of our bodies at this level will reshape how we diagnose, treat, and ultimately, prevent life-threatening illnesses.