Expanding HPV vaccination programs to include young men is crucial for achieving herd immunity and eliminating HPV-related cancers, including cervical cancer, which claims over 300,000 lives annually worldwide. New research from the University of Maryland demonstrates that relying solely on female vaccination is insufficient in many countries, and that vaccinating boys significantly improves the feasibility of eradication.
The Problem with Gender-Biased Vaccination
For years, HPV vaccination has been primarily marketed towards women as a preventative measure against cervical cancer. While this approach has dramatically reduced cervical cancer rates – with some regions seeing a nearly 90% drop in cases over the past two decades – it overlooks the broader impact of the virus. HPV isn’t just a women’s health issue. Men are at risk of HPV-linked cancers, including anal, penile, and head and neck cancers, and play a vital role in viral transmission.
This skewed focus has led to significant disparities in vaccination rates, with far fewer young men receiving the vaccine compared to women in many nations. In South Korea, for example, current female vaccination rates are at 88%, still short of the 99% needed for herd immunity. Without broader coverage, HPV will continue to circulate and cause preventable deaths.
Mathematical Modeling Shows the Way Forward
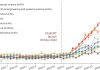
Researchers developed a new mathematical model calibrated using South Korean cancer data to assess the impact of different vaccination strategies. Their findings are clear: vaccinating 65% of boys in South Korea, alongside maintaining current female vaccination rates, could achieve herd immunity. Even if female vaccination rates were to drop slightly to 80%, reaching 80% coverage among males would still allow for cancer elimination.
This is because vaccinating boys reduces the overall pressure to achieve extremely high female coverage. The virus spreads through sexual contact and skin-to-skin transmission, meaning men can both contract and spread HPV. If a large percentage of the male population is immune, the virus has fewer hosts to infect, protecting both genders.
Global Implications and Future Goals
The model’s principles apply beyond South Korea. Researchers estimate that approximately 70% coverage among both men and women in the US would be sufficient for herd immunity. If these vaccination strategies were scaled up globally, scientists predict the elimination of cervical cancer in 149 out of 181 countries by the end of the century.
The study’s authors recommend vaccinating boys aged 12–17 alongside girls and older women who may have missed earlier vaccination opportunities. Recent evidence suggests that vaccinating older individuals can still provide some protection. With widespread vaccination and continued cervical screenings, we can prevent an estimated 350,000 annual deaths from cervical cancer worldwide. The path to eradication is clear: gender-inclusive vaccination policies and a commitment to protecting all populations at risk.